Journey to the ICU- Levels and ICU Categorization
- Miki Shibata

- May 31, 2019
- 4 min read
Updated: Jun 1, 2019

Author: Miki Shibata, MS, CCC-SLP Edited by: Ainsley Martin, MS, CCC-SLP
“If you know the enemy and know yourself, you need not fear the result of a hundred battles. If you know yourself but not the enemy, for every victory gained you will also suffer a defeat. If you know neither the enemy nor yourself, you will succumb in every battle.”
― Sun Tzu, The Art of War
I’m not afraid to admit that I’ve been intimidated by intensive care units and critical care teams. My first time in the ICU on my own, I remember being stunned by the incredibly frail-looking patients, and super curt interactions that I had with nurses and the providers. I really felt this strong fear that I better shape up or I can lose respect really fast, or worse endanger a patient.
In ICU the pace is fast, the language precise. Patients are critically ill and tenuous, and plan of care changes all the time as a patient’s medical status fluctuates. One day is never the same as the next. And all the lines, tubes, drains, and beeping machines can be overwhelming.
However, I now absolutely love the ICU- it’s our chance as medical speech-language pathologists to make first-line contributions to a patient’s care as a part of the multidisciplinary team. If you are considering pursuing a career in critical care, dipping your toes into the ICU, or just wanting to gain more information, you’re in the right place!
In order for a speech pathologist to navigate critical care and intensive care units and is first important to know what an ICU is, understand the different levels and categorizations of ICUs, and have a general knowledge of the key players, patients, goals, and resources available.

We all think we know the ICU...but do we really?
Luckily the World Federation of Societies of Intensive and Critical Care Medicine convened a task force to define the ICU and develop a system of categorization based on the intensity of care provided.
“An ICU is an organized system for the provision of care to critically ill patients that provides intensive and specialized medical and nursing care, an enhanced capacity for monitoring, and multiple modalities of physiologic organ support to sustain life during a period of life-threatening organ system insufficiency. Although an ICU is based in a defined geographic area of a hospital, its activities often extend beyond the walls of the physical space to include the emergency department, hospital ward, and follow-up clinic.” (Marshall, et al., 2017)
Let that soak in.
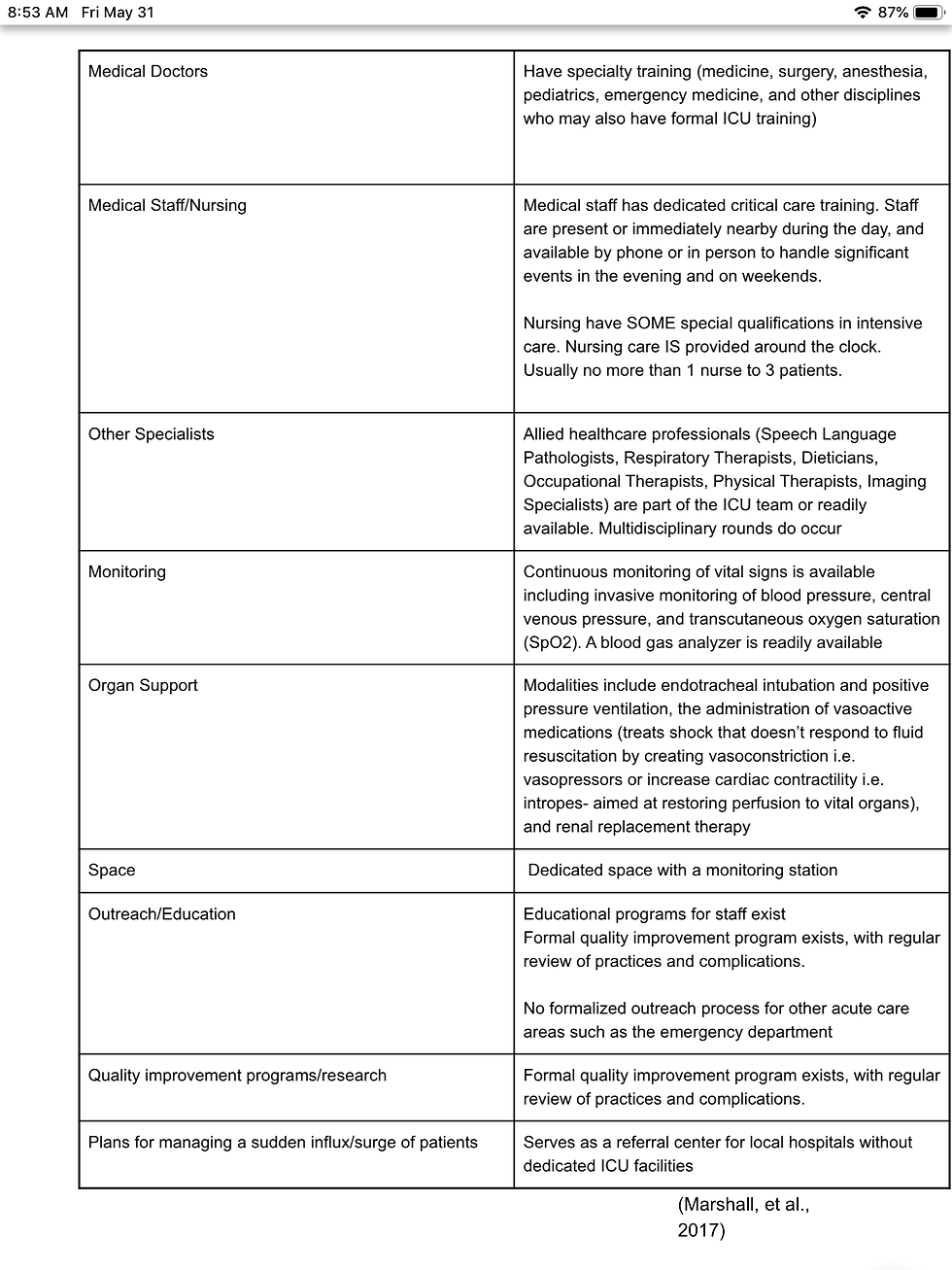
So ,an ICU is differentiated from other units in the hospital by;
the level of staff training
the intensity of care (less patients per RN or Physician)
the monitoring capabilities
the capability for organ support
the knowledge/skills available as a consult service to other departments/units in the hospital
As speech pathologists working in acute care, it is vital that we research and understand the elements that make the ICU an ICU to better serve our patients and make meaningful contributions as part of the medical team.
Now, the need for categorization or stratification of ICUs exist because as you all may know, not all ICUs have the same capacities. So the same task force also introduced three categories/levels of ICUs;
Level I Primary ICU

Level II Secondary ICU
Level III Tertiary ICU

What are the different types of ICUs?
Trauma ICU - Monitoring/care for patients that suffered blunt or penetrating trauma (e.g. motor vehicle accidents, gunshot wounds, mechanical falls)
Surgical ICU - Monitoring/care for pre or post surgical patients (e.g. open heart/lung/ gastrointestinal/cardiovascular procedures...I’ve also seen post laryngectomy patients in this unit as well )
Medical ICU- Monitoring/care for wide-array of “medicine” patients ranging from pulmonary, gastrointestinal, hematic conditions
Cardiac/Coronary Care Unit (CCU) or Cardiovascular ICU (CVICU) - management of diseases/surgeries related to the heart e.g. complications from acute myocardial infarctions (heart attacks), cardiogenic shock, post-infarction angina (ischemic chest pain exhibited at rest or with minimal activity, 24 hrs or more after an acute myocardial infarction), congestive heart failure. Vascular diseases seen include aortic dissection, aortic aneurysm, peripheral artery disease (Kasaoka, 2017)
Neuro ICU - Monitoring care for complications arising from neurological conditions such as encephalopathic (brain disease, damage, or malfunction)patients, the control of intracranial pressure/ICP (brain injury or other health issues can cause a buildup of pressure inside the skull), respiratory/autonomic (system that controls heart rate, digestion, respiratory rate, pupillary response, urination, and sexual arousal)/bulbar (cranial nerves 9- glossopharyngeal, 10- vagus, 11-spinal accessory, 12- hypoglossal) insufficiency, and the results of severe neuromuscular debilitation. Diagnoses treated may include: strokes, spinal cord lesions, status epilepticus, acute bacterial meningitis etc. (Howard, et. al, 2003)
Neonatal ICU - Monitoring and managment of critically ill newborns including those born premature, those born with or those who develop neurological/cardiac/respiratory/blood sugar regulation issues.
So when you’re looking for your next ideal setting, hop onto the hospital website and see what level of ICU they offer, and make sure to take CEUs/ask for more orientation if you feel like you need to brush up on your knowledge or skill set. And of course, stay tuned for upcoming posts as part of our Journey to the ICU series!
References:
Howard, R. S. (2003). Admission to neurological intensive care: Who, when, and why? Journal of Neurology, Neurosurgery & Psychiatry, 74(90003), 2iii-9. doi:10.1136/jnnp.74.suppl_3.iii2
Kasaoka, S. (2017). Evolved role of the cardiovascular intensive care unit (CICU). Journal of Intensive Care, 5(1). doi:10.1186/s40560-017-0271-7
Marshall, J. C., Bosco, L., Adhikari, N. K., Connolly, B., Diaz, J. V., Dorman, T., . . . Zimmerman, J. (2017). What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. Journal of Critical Care, 37, 270-276. doi:10.1016/j.jcrc.2016.07.015
Stanford Children’s Health. Neonatal Intensive Care Unit. Retrieved May 25, 2019, from https://www.stanfordchildrens.org/en/topic/default?id=the-neonatal-intensive-care-unit-nicu-90-P02389




This post offers a raw and deeply human glimpse into the emotional toll on ICU staff during COVID-19. It highlights the intense stress, resilience, and silent sacrifices that go unseen by the public. Such narratives remind us of the psychological weight borne by frontline workers and the importance of empathy and support for those navigating these high-press